Shaping better health for everyone
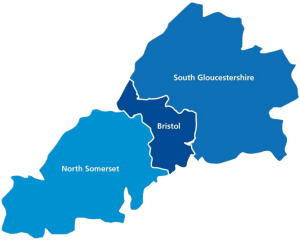
The Bristol, North Somerset and South Gloucestershire Integrated Care Board (ICB) was established on 1 July 2022. We’re responsible for developing plans to meet the health needs of our population, managing the NHS budget and arranging for the provision of health services in our area.
Our work is focused on four key aims:
- Improving outcomes in population health and healthcare
- Tackling inequalities in outcome, experience and access
- Enhancing productivity and value for money
- Helping the NHS support broader social and economic development

It has been another exceptional and busy year during which we moved on from the Clinical Commissioning Group model to launch the new Integrated Care Board (ICB).
This year we have really focussed on getting the foundations of our ICB right so that we can achieve our purpose of improving outcomes in population health and healthcare; tackling inequalities in outcomes, experience and access; enhancing productivity and value for money and supporting broader social and economic development.
In this Annual Review, we’ve highlighted some great work delivered in our first year. For example, there is information about our high uptake of annual health checks for people with learning disabilities as well as information on the innovative Care Traffic Co-ordination Centre, which is helping us to anticipate and respond to pressures in our health and care system in real time.
You can also see our annual review and accounts in full from our first nine months as an Integrated Care Board, as well as our final three months as a Clinical Commissioning Group.

Our health and care system in numbers
1 million
Population

50,000+
Health and care staff

76
GP practices

2
Acute hospitals

1
Ambulance trust

1
Community provider

1
Mental health trust

3
Councils

1000s
of voluntary organisations

Tackling inequalities
Integrated Care Boards have a duty to reduce inequalities, both in people’s ability to access health services and in the outcomes achieved for them by those services.
During 2022/23, we continued the work started by our predecessor organisation, Bristol, North Somerset and South Gloucestershire CCG, to reduce health inequalities. We’re committed to advancing equality and reducing health inequalities for our diverse population and in the summer of 2022, we led a system-wide population health needs assessment, called ‘Our Future Health’. The report sets out the key issues and inequalities faced by our communities and has been central to the development of our health and wellbeing strategy.

Health and care staff winter vaccination film
In winter 2021/22, our data showed a disparity of up to 30% in uptake of flu and Covid-19 vaccination among health and care staff from some Minority Ethnic communities. In response, BNSSG’s Covid-19 Vaccination Programme team produced a cross-system film in winter 2022/23 to encourage workforce vaccination, supported by colleagues from across our organisations.
Staff members shared their personal reasons for getting vaccinated in order to encourage colleagues to do the same. People were filmed in their place of work in a wide range of roles, with Black and Minority Ethnic staff members strongly-represented. Each organisation used the film, internally, as part of their winter resilience work and we made a public-facing version for social media. NHS England also adapted the film as part of a national digital campaign. The film will be updated and reused this winter, 2023/24.
Urgent care multilingual guidance
Our insight suggests that most people are keen to use the correct NHS service for their needs and recognise the benefits of doing so. However, many are uncertain about their options and unsure where to go for help. This is often particularly true for people whose first language is not English, and especially those who may not have had previous experience of the UK health system.
To help people understand their options and promote equitable access to services, we published a concise, multilingual guide to local services. This was distributed directly to households in areas associated with higher Emergency Department admissions for minor, non-emergency conditions. The leaflets were supported by a local promotional campaign in health and care settings such as GP practices and Emergency Departments. It’s a simple solution to people’s information needs which is helping to ensure equitable access to services, for everyone we serve.
Learning disability health checks
People with learning disabilities are some of the most vulnerable in our area, often having poorer physical and mental health outcomes and shorter lives compared to others.
Part of the reasoning for this is that people with a learning disability do not always know when they are ill or need to see a doctor. That’s why everyone with a learning disability over the age of 14 is offered an annual health check.
We are proud that, for the third year running, our area has achieved the national standard in uptake of health checks for people with learning disabilities, with an 82% uptake rate against a target of 75%. In addition, health action plans are in place for 98% of those people.
Listening to you
We’re committed to involving local people in the design and development of services.
Across our integrated care system, and as an ICB and a partnership, we are clear that the communities we serve – the people we provide health and care services for – are at the heart of all that we do. By understanding our population we can focus on, and prioritise, the issues of greatest importance: their health and care needs, and what helps to keep them happy, health and well.

Have Your Say
In the summer of 2022, we asked members of the public what keeps them happy, healthy and well across Bristol, North Somerset and South Gloucestershire. The engagement exercise was to help us be informed and shape our Integrated Care System (ICS) Strategy. We also encouraged our local communities to take part in our Have Your Say survey to learn more about their health needs to help shape our NHS health services and to close the health inequalities gap.
The listening and engagement exercise saw over 3,000 responses, collecting more then 21,000 comments, and held 50 community events.
The results of Have Your Say survey, the full report, and videos of local people talking about what keeps them happy, healthy and well can be found on the Healthier Together website.

Culturally sensitive child flu vaccination Information
After feedback from Minority Ethnic communities that some parents did not want their children to have the nasal flu vaccine as it contains a pork derivative, our Covid-19 Vaccination Programme adapted national resources to include mention of the injectable vaccine which has no porcine content.
We worked with community interest company, Caafi Health, to create audio and written translations in six languages to support people who are not literate in their spoken language. These short videos launched in winter 2022/23 and are designed to be shared in WhatsApp groups to provide trusted information for parents who might not be able to access the content in other formats.

Weston insights campaign
In early 2023, we ran a campaign in central Weston-super-Mare based on local vaccination data and insight gained from qualitative research we conducted with unvaccinated people living in areas of multiple deprivation with a predominantly White British population. The campaign had three phases: Listen, in which we asked people to tell us the questions they had about Covid; Inform, where we provided the answers to the top questions people in Weston told us they had; and Deliver, where we provided an opportunity for vaccination at Community Health Events, alongside other health and wellbeing services in response to what people told us.
We identified a huge opportunity for our health system and the voluntary and community sector to work together to make access to health and wellbeing services easier for underserved communities. The insights we gained will inform new models of partnership working for future vaccination and health initiatives.

Citizens’ Panel
Our Citizens’ Panel supports regular surveys and ad-hoc research projects to help us improve health and care in our area. The panel is made up of more than 1,500 members from across Bristol, North Somerset and South Gloucestershire.
In 2022/23 we ran three surveys on a range of topics including NHS 111, urgent care behaviours, system strategies, future priorities and what keeps our population healthy and well.
The panel provides us with a deeper understanding of what our population needs and wants, helping us to shape and influence our plans for future health and care services.
The results from the surveys are shared with colleagues across the Integrated Care System, on our Healthier Together website and with our panel members.
View the latest Citizens' Panel survey results
Transforming services
We work with our partners to deliver long-term strategic transformation programmes which ensure services continue to meet people’s needs now and in the future.
Our transformation priorities are guided by our health and care system Strategy and our ICB’s Joint Forward Plan. This sets out how the ICB will deliver on the national vision of high-quality healthcare for all. During 2022/23 we made good progress on a range of large-scale transformation programmes, working with our partners.

NHS@Home
NHS@Home is a partnership service involving NHS healthcare providers from across Bristol, North Somerset and South Gloucestershire. The service helps people to get the care they need at home safely and conveniently, providing an alternative to being in hospital.
NHS@Home uses a mixture of digital monitoring and face-to-face visits from specialist teams. Individuals receiving care use equipment contained in a so-called ‘Doccla Box’ to monitor their own health. This data is then sent to healthcare professionals for evaluation at the clinical hub in Bristol.
NHS@Home can currently care for up to 165 people in our area at any one time, which means an increase in bed capacity and reduced pressures in hospitals, and improved care for the local community. The service was successfully implemented during the Covid-19 pandemic and has now been enhanced to support those with other conditions, such as respiratory and heart conditions.
Since 2021, NHS@Home has provided an alternative to admission or supported earlier discharge a total of 4032 times. During this time, the service has supported local people to be cared for at home for an additional 38,760 days.
NHS@Home was featured on BBC Points West and ITV West Country.
Find out more about NHS@Home
Population Health Management
Population Health Management (PHM) is the way we work together to understand and improve the health of people and communities using joined-up health and social care data.
It can be used by everyone working in health care, supporting the ICB and wider health and care organisations to develop news services and improve current services, enabling us to provide the best care for local people.
PHM supported 30 projects across a range of areas within health in Bristol, North Somerset and South Gloucestershire in 2022-23.
A project that has benefitted from PHM is the Healthy Hearts Group in Bristol’s Inner City area, which supported 102 people at-risk of heart failure.

Mental Health Integrated Urgent Care ‘Front Door’
During the year we worked with a range of partners including BrisDoc, Avon and Wiltshire Mental Health Partnership Foundation Trust and South Western Ambulance Service NHS Foundation Trust – and police, fire and voluntary organisations – to implement an integrated urgent and emergency care ‘front door’ service across 999 and 111 for people in mental health crisis.
The service provides three layers of intervention and trusted onward referrals to support any person presenting with mental health needs to 999 or 111, providing remote advice through a multidisciplinary mental health team or a rapid face-to-face response through a network of ‘mobile pods’ across the area.
This initiative was Highly Commended in the HSJ Patient Safety Awards and also received a regional NHS Parliamentary Award.

Building our system
We’re working with our partners to join up services around individuals, with a structure that focuses on the unique needs of our local communities
Our ability to stay healthy and well depends on a range of things, including social connections, employment, housing, and education. To make a real difference in people’s lives, health and care services need to reflect the importance of these wider factors and the role they play in our health and wellbeing. To help do this, we’ve established six Locality Partnerships made up of local health, social care, and voluntary sector organisations – with citizens and community as equal partners. The Partnerships work as one team to understand what matters most for their community and improve services in a way that puts people at the heart of every decision.

Getting to know our localities
Two of our Locality Partnerships, One Weston and Woodspring, have introduced a podcast to enable colleagues from voluntary sector, social care and health providers better appreciate one another’s role in supporting people to stay healthy and well.
David Moss, Head of Locality for One Weston Locality Partnership, hosts the podcast to understand more about who the staff working in local health and care services are, what motivates them, the challenges they face and how it feels to work where they work.
There are 10 podcasts so far featuring a variety of guests including Director of Public Health at North Somerset Council, Matt Lenny; Chief Officer of Citizens Advice North Somerset, Fiona Cope; and our Chief Executive Shane Devlin. Each podcast explores a different topic ranging from the cost of living crisis to helping people live as well as they can.
You can listen to the podcasts on Buzzsprout, Apple, Spotify or your chosen podcast platform.
Health leaders from New Zealand recently visited Bristol as part of an international study tour to find out more about the collaborative work of Woodspring Locality, one of the two Locality Partnerships in North Somerset. Watch a video from the visit on our YouTube channel.
Read more about the North Somerset Partnership Podcast
Care traffic co-ordination centre
We’ve also been working hard to build our system by joining up health and care services that span the wider BNSSG area. This work includes our new ‘intelligent care traffic co-ordination centre’, which was launched in 2023. The centre brings together data on capacity and demand in ambulance services, NHS 111, hospital services, social care, GP and mental health providers and helps partners work together to maintain services across our whole system.
The data system at the heart of the new centre uses artificial intelligence to analyse and forecast demand for services in real time, helping us to anticipate and pre-empt capacity issues before they take place. For health and care partners, the centre will mean much more efficient use of our resources and better service performance, with reduced waiting times and more timely discharge from our hospitals. For local people, it will mean better-informed care plans, an improved experience of services and better health outcomes.

Improving services
We’re committed to a culture of continuous improvement and enhancement to services.
We work with system partners to monitor how services perform and make enhancements and improvements to make sure they continue to meet the needs of local people. During the last year we’ve continued to invest in improvements to a range of services including our system Clinical Assessment Service and our Orcha library of self-help apps for local people.

System Clinical Assessment Service
We’ve enhanced our NHS 111 service to help more people access urgent care in a timely way without needing to go to the Emergency Department (ED) or an urgent care centre. The system Clinical Assessment Service (CAS) is a multidisciplinary team of healthcare professionals who work alongside 111 to assess and advise people who’d normally be referred to ED or 999 for assessment. In many cases, this assessment – and the medical advice and guidance that people need – can be delivered via a telephone or video consultation, with any prescriptions transmitted directly to the patient’s pharmacy for collection.
This ‘clinical validation’ of the most urgent patients is helping reduce ED attendances and improving the service we provide for local people. The proportion of eligible patients who received clinical validation via the system CAS rose from 64% in April 2022, to 81% in February 2023.
Green social prescribing
Studies have shown that regular access to green and ‘blue’ spaces can offer a range of health benefits including reducing stress, sadness and isolation and promoting social interaction.
In our area, we’ve been pioneering a new way to help people access the mental health benefits of their natural environment, with healthcare professionals able to refer people into a wide range of community activities including gardening, nature appreciation, walking groups and even open water swimming.
As a national ‘test and learn’ site for Green Social Prescribing, we’ve focused in particular on improving access for communities hardest hit by coronavirus, such as those living in deprived areas, people with mental health conditions or BAME communities.
The programme has supported more than 3000 people across 60 activities. Outcome analysis looked at people’s low happiness and high anxiety scores before and after the programme. It showed reduced levels of high anxiety (from 57% to 27%) and reduced levels of low happiness (from 43% to 19%).
ORCHA App library
The Bristol, North Somerset and South Gloucestershire Organisation for the Review of Care and Health Apps (ORCHA) Library is an exciting development that is helping local people to self-care and manage a range of existing conditions.
The ORCHA Library has a range of apps available on health and wellbeing such as mental health, fitness and nutrition. People with long-term issues can also benefit from a range of apps within the library on diabetes, cancer care, fibromyalgia, multiple sclerosis and more. It can also provide advice to parents on managing minor childhood illnesses. The search function helps people to search for appropriate apps and links to download through Android and iPhone devices.
In May 2023, 421 healthcare professionals logged into the ORCHA Library. 25,379 webpages were viewed, and 54 recommendations were made by clinicians to their patients.
The ORCHA Library aims to support people digitally and provide them with clinically approved information. Visit the ORCHA Library to see the apps that are currently available.